What is an Epidural Steroid Injection (ESI)?
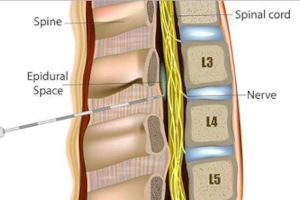
An Epidural Steroid Injection (ESI) is a common pain management technique used to treat chronic pain conditions associated with the spinal nerves. The procedure involves the injection of corticosteroid medication into the epidural space of the spine, which is the area surrounding the spinal cord and nerve roots. This space is targeted because it's often where inflamed nerve roots are located, causing pain and discomfort. Corticosteroids help reduce inflammation and swelling of the nerves, leading to decreased pain, improved mobility, and a significant reduction in other symptoms such as numbness or tingling in the legs or arms. ESIs are particularly effective for conditions like herniated discs, spinal stenosis, and radiculopathy.
The process of administering an ESI is minimally invasive and typically performed under local anesthesia with fluoroscopic (X-ray) guidance to ensure accuracy. Patients can often return to their normal activities shortly after the procedure, with pain relief that can last from weeks to months, varying from person to person. While ESIs are a valuable tool in the management of spinal-related pain, they are usually part of a comprehensive treatment plan that may include physical therapy, medication, and lifestyle modifications. This approach allows for targeted pain relief while also addressing the underlying causes of pain, offering a holistic strategy to managing chronic spinal conditions.
What are the benefits and risks of an Epidural Steroid Injection?
Epidural Steroid Injections (ESIs) are a common treatment for chronic pain, particularly in the lower back and neck. They offer several benefits but also carry certain risks:
Benefits
- Pain Relief: ESIs can provide significant relief from pain caused by inflammation, herniated discs, spinal stenosis, or radiculopathy. This relief can improve quality of life and functionality, allowing patients to participate more fully in physical therapy and other rehabilitative activities.
- Minimally Invasive: Compared to surgery, ESIs are less invasive, have a lower risk of complications, and typically require no significant downtime.
- Diagnostic Value: By targeting specific areas of the spine, ESIs can help pinpoint the exact source of pain, providing valuable diagnostic information.
- Delaying Surgery: For some patients, the relief provided by an ESI can postpone or even eliminate the need for spinal surgery.
Risks
- Infection: As with any procedure that breaks the skin, there is a risk of infection, including serious infections such as meningitis or abscesses.
- Dural Puncture: Accidental puncture of the dural sac can occur, potentially leading to a headache that requires treatment.
- Nerve Damage: Though rare, there is a risk of nerve damage, which could result in increased pain, numbness, or weakness.
- Side Effects from Steroids: Systemic effects from the steroid medication, including weight gain, elevated blood sugar, decreased immune response, and mood swings, can occur, especially with repeated injections.
- Temporary Increase in Pain: Some patients experience a temporary increase in pain following the injection before the pain-relieving effects of the steroids take hold.
Schedule a consultation with us if you are considering an ESI. We will have a detailed discussion with you about the potential benefits and risks, taking into account your specific health condition, pain severity, and treatment goals.
Who is a good candidate for an Epidural Steroid Injection?
Good candidates for an Epidural Steroid Injection (ESI) are individuals experiencing chronic pain due to spinal conditions that have not adequately responded to conservative treatments. These conditions often include herniated discs, spinal stenosis, radiculopathy (nerve pain), and sciatica, which cause inflammation and pain in the spinal nerves. Ideal candidates typically exhibit the following criteria:
- Clear Diagnosis: Patients with a clear diagnosis of a spinal condition causing nerve root irritation or inflammation, confirmed through diagnostic imaging like MRI or CT scans.
- Conservative Treatment Failure: Those who have tried and not found sufficient relief from non-invasive treatments such as physical therapy, medications, or lifestyle modifications.
- Moderate to Severe Pain: Individuals suffering from moderate to severe pain that impacts their quality of life, daily activities, and ability to work or engage in physical activities.
- No Immediate Need for Surgery: Patients for whom surgery is not immediately necessary, or who wish to delay or avoid surgical intervention for their spinal condition.
- No Contraindications: Absence of conditions that contraindicate the procedure, such as active infections, bleeding disorders, or allergies to the injection components.
ESIs are considered a middle-ground option for pain management, providing relief when conservative methods have failed but before more invasive surgical options are considered. Consult with us for a thorough evaluation to determine if an ESI is the most appropriate treatment option for an your specific situation.
How is an Epidural Steroid Injection (ESI) performed?
The process involves the following steps:
Preparation
- Patient Assessment: A thorough review of the patient's medical history and imaging studies to confirm the diagnosis and identify the specific spinal level for injection.
- Informed Consent: The patient is informed about the benefits, risks, and alternatives to the procedure, and consent is obtained.
- Positioning: The patient is positioned to allow easy access to the epidural space, usually lying face down on an X-ray table.
The Procedure
- Sterile Technique: The skin over the injection site is cleaned with antiseptic solution to minimize infection risk, and the area is covered with sterile drapes.
- Local Anesthesia: A local anesthetic is applied to numb the skin and tissue down to the epidural space, reducing discomfort during the procedure.
- Fluoroscopic Guidance: Fluoroscopy, a type of real-time X-ray, is used to guide the needle accurately into the epidural space. Contrast dye is often injected to confirm the correct placement of the needle.
- Steroid Injection: Once the needle is properly positioned, a corticosteroid solution, often mixed with a local anesthetic, is injected into the epidural space to reduce inflammation and pain.
- Monitoring: After the injection, the patient is monitored for a short period for any adverse reactions. Most procedures are done on an outpatient basis, allowing the patient to go home the same day.
Post-Procedure
- Recovery: Patients are advised to rest for the remainder of the day and can usually resume normal activities the following day, with potential restrictions on driving and strenuous activity for a short period.
- Follow-up: The effectiveness of the injection is assessed in follow-up appointments, and additional injections may be recommended if the response is favorable but incomplete.
The ESI aims to reduce pain and inflammation, providing relief that can last from weeks to months. This procedure is part of a comprehensive pain management plan, which may include physical therapy, medications, and lifestyle modifications to address the underlying cause of pain.